Bronchopulmonary dysplasia is the term devised to describe chronic lung changes that developed in premature infants with surfactant deficiency treated for respiratory distress syndrome (RDS). BPD was considered a disorder of lung and airway injury and repair primarily due to barotrauma and oxygen toxicity.
With improving management techniques, younger and lower birth weight infants are now surviving, but are born at increasingly immature stages of lung development. Therefore, despite major advances in treatment, the overall incidence of chronic lung disease of prematurity (defined at 36weeks of postmenstrual age) has not significantly changed over time. The clinical definition and radiographic features have evolved and it is now considered a multifactorial disorder of disrupted alveolar growth and pulmonary angiogenesis. 40% of babies <28wks develop CLD. The majority survive with gradual weaning off oxygen and often normalization of radiographs by 1-2yrs. There are however often long-term sequelae including pulmonary hypertension in ~25%, increased susceptibility to respiratory infection, tracheobronchomalacia, asthma and emphysema as well as neurodevelopmental delay and growth failure.
Imaging, especially chest radiographs, are important in managing and following these infants. Chest CT is useful in more complex cases and to evaluate the extent and severity of disease and complications such as pulmonary hypertension, acquired pulmonary vein stenosis and emphysema. Neuroimaging may also be needed for diagnostic and prognostic reasons.
|
|
 |
 |
|
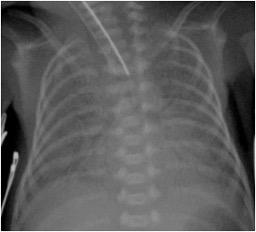
24 week gestation infant CXR on day 1with the diffuse granular “ground glass” pattern of respiratory distress syndrome of prematurity (surfactant deficiency disease) |
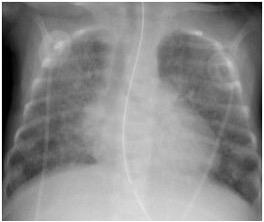
12 weeks of age CXR with changes of chronic lung disease characterized by heterogeneous cystic lucencies separated by coarse reticulations, reflecting regions of air trapping and early septal fibrosis. |
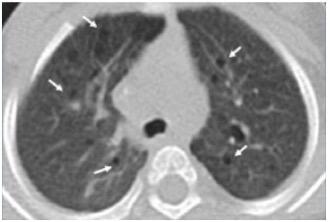
16 months of age Axial CT on lung window shows changes of chronic lung disease on non-contrast CT characterized by numerous small cyst-like lucencies (arrows) and mild diffuse lung haziness. |
 |
 |
 |
|
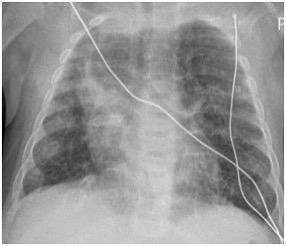
Chest XR 5 months 28 week gestation infant with intrauterine growth retardation. Chest radiograph shows an enlarged cardiac silhouette, hyperinflated lungs, reticulation, cyst-like lucencies, and bands of density consistent with chronic interstitial disease. There is also emphysema of the left upper lobe herniating across midline. |
5 months Axial noncontrast CT shows features of an alveolar growth disorder with overinflated lung lobules and interspersed fibroproliferative changes.
|
10 months Axial noncontrast CT shows evolution to air trapping/emphysema with less reticular change. There is bibasilar atelectasis. The fact that this baby had IUGR helps explain the severity of CLD in a relatively more mature infant.
|
References:
1. Northway NEJM 1967 Pulmonary disease following respirator therapy of hyaline- membrane disease. Bronchopulmonary dysplasia
2. Northway NEJM 1990 Late pulmonary sequelae of bronchopulmonary dysplasia
3. Howling, Northway AJR 2000 Pulmonary sequelae of bronchopulmonary dysplasia survivors4. 4. 4.Merritt Sem fetal neonatal med 2009 The “new” bronchopulmonary dysplasia: challenges and commentary
5. Tracy, Cornfield Current opinion in pediatrics 2017 The evolution of disease: chronic lung disease of infancy and pulmonary hypertension
6. Swier Am J perinatology 2016 Pulm vein stenosis in neonates with severe bronchopulmonary dysplasia
7. Agrons GA Radiographics 2005 Lung disease in premature neonates: radiologic-pathologic correlation
8.Parad RB Ped Rad 2012 Update on the diagnosis & management of bronchopulmonary dysplasia/chronic lung disease of infancy: what the radiologist should know