Vasculitis is characterized by the inflammation of blood vessels, and its underlying cause is often unclear. The incidence of vasculitis is approximately 23 cases per 100,000 children annually. This condition presents with a wide range of symptoms, making diagnosis challenging. Furthermore, the symptoms and laboratory markers associated with vasculitis are often nonspecific. Therefore, imaging plays a critical role in assessing the extent of the disease and identifying potential complications.
When considering imaging for vasculitis, the focus depends on the size of the affected blood vessels. For large to medium-sized vessels, imaging aims to directly visualize the inflamed vessel wall. In contrast, for medium to small-sized vessels, the emphasis shifts to evaluating end-organ complications. Various imaging modalities are employed in the diagnosis and management of vasculitis, including magnetic resonance imaging (MRI), positron emission tomography combined with MRI (PET/MRI), computed tomography (CT), positron emission tomography combined with CT (PET/CT), and ultrasound (US). However, it is important to note that ultrasound may underestimate the true extent of the disease.
Example: Takayasu arteritis
| CT |
 |
| MR |
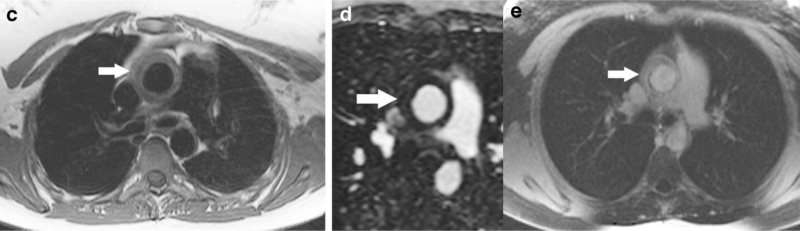 |
| PET/MRI |
 |
Example: Kawasaki Disease
 |
 |
 |
Example: IgA vasculitis imaging US

Example: Granulomatosis with polyangiitis CT

